A clinical examination, suspect image or abnormal biological result may require a patient to consult a specialist who, if necessary, will perform additional examinations to either reject or confirm a cancer diagnosis.
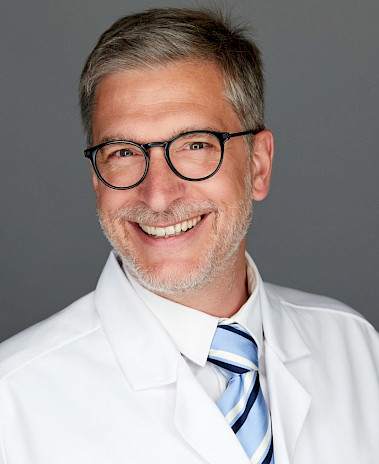
A multidisciplinary conference (Tumour Board), brings together all the specialists involved in the oncology treatment pathway, these are radiology, pathology, nuclear medicine, surgical oncology, medical oncology, radiotherapy, plastic and reconstructive surgery, etc., each specific case is examined in detail and the best possible treatment strategy is discussed and established.